Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

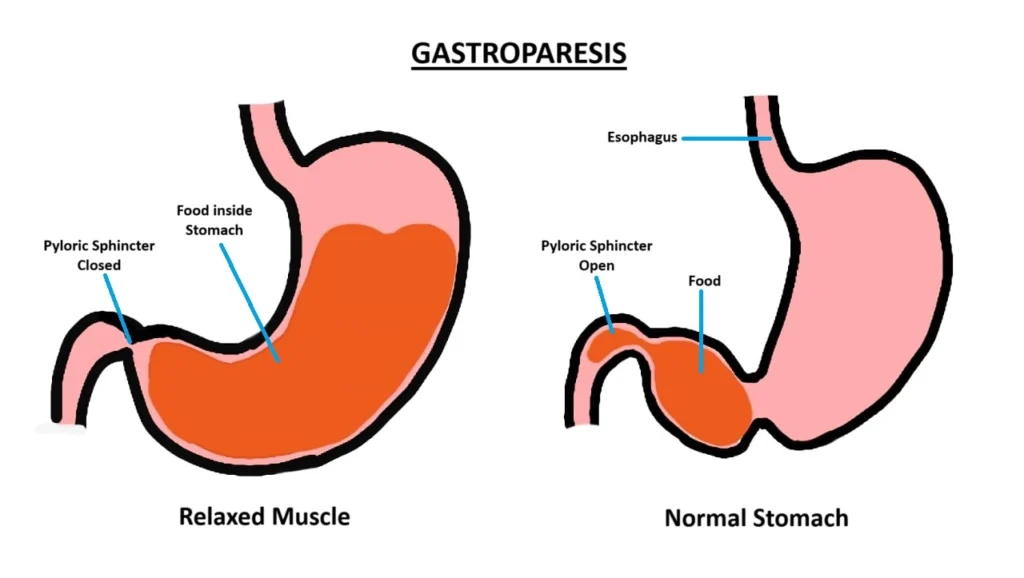
Gastroparesis is a chronic digestive disorder where the stomach’s ability to empty food into the small intestine is slowed down or impaired. This condition occurs when the muscles in the stomach, which are supposed to contract and push food through the digestive tract, don’t function properly due to nerve damage or other underlying factors. As a result, food lingers in the stomach longer than it should, leading to a range of uncomfortable symptoms.
Gastroparesis, a condition marked by delayed gastric emptying, impacts a diverse group of people, but certain demographics are notably more affected. Understanding these groups helps to better address the challenges of managing and treating this complex disorder.
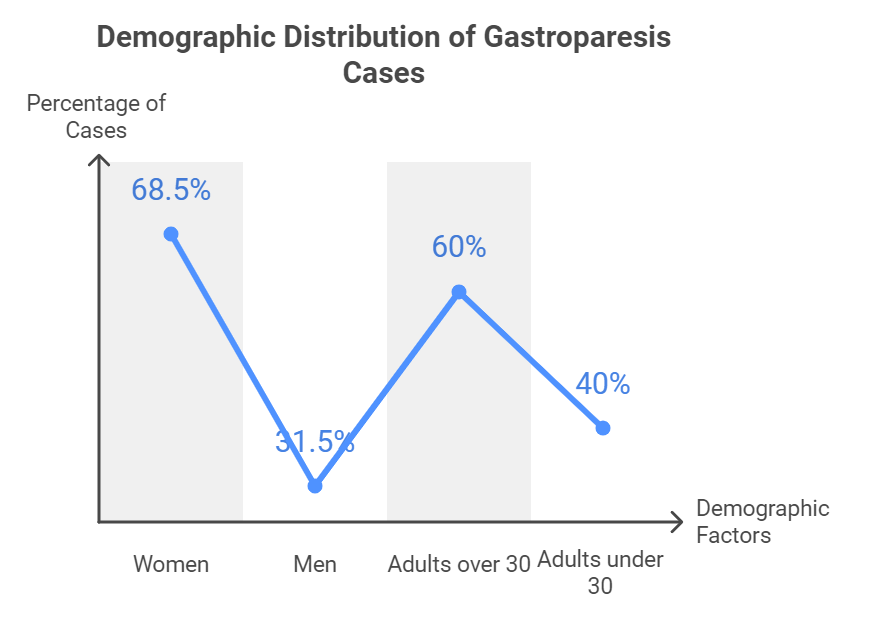
Gastroparesis disproportionately affects women, with studies revealing that approximately 68.5% of those diagnosed are female. This significant gender gap suggests that hormonal differences or other gender-specific factors may play a role, although the precise reasons remain under investigation.
While gastroparesis can develop at any age, it is most commonly observed in adults over 30 years old. The incidence tends to rise with age, likely due to the cumulative impact of risk factors such as diabetes and a history of abdominal surgeries. Younger individuals can also be affected, but they are less common cases.
When looking at gastroparesis across different ethnic groups, Caucasians appear to be the most commonly affected demographic. However, recent studies highlight that a significant portion of patients also come from South Asian and East Asian backgrounds, particularly individuals of Indian, Pakistani, Bangladeshi, and Chinese descent.
This emerging data suggests that while gastroparesis might appear more frequently in Caucasian populations, it’s important to acknowledge its impact on a broader range of ethnicities. Understanding these patterns can aid in creating more culturally sensitive approaches to diagnosis and treatment.
Several health conditions notably increase the risk of developing gastroparesis:
Recent data indicates that gastroparesis affects approximately 267.7 per 100,000 adults in the U.S., underscoring its significance as a public health concern. The condition’s prevalence highlights the need for increased awareness and more effective management strategies.
By focusing on these demographics, healthcare providers can tailor their approach to treatment and support, ensuring that individuals who are most at risk receive the care they need.

Recent research on gastroparesis has unveiled several crucial insights and advancements in the understanding, diagnosis, and management of this condition. Here’s a summary of key studies and their contributions:
This study introduces groundbreaking advances in our comprehension of gastroparesis, particularly highlighting the role of smooth muscle cells and interstitial cells of Cajal as the stomach’s pacemaker units.
It showcases new diagnostic tools such as wireless motility capsules and carbon-13 labeled breath tests, and novel therapies like gastric peroral endoscopic pyloromyotomy (G-POEM). These developments aim to offer more tailored and effective management strategies for patients.
Utilizing a large U.S. national claims database, this research provides valuable real-world evidence on the prevalence and treatment outcomes of gastroparesis.
It underscores the prevalence rates and associated comorbidities, highlighting the need for enhanced diagnostic accuracy and treatment methods in clinical practice.
This review synthesizes recent findings on the pathophysiology of gastroparesis, with a focus on intrinsic neuropathy as a significant factor.
It discusses validated diagnostic tests such as 99-Technetium scintigraphy and the 13C breath test, as well as therapeutic strategies ranging from dietary adjustments to surgical interventions for severe cases.
This global study reveals that gastroparesis-like symptoms (GPLS) are widespread, particularly among individuals with diabetes.
It assesses their impact on quality of life and healthcare utilization, emphasizing the need for improved recognition and management of these symptoms in clinical settings.
A UK-based population study offers insights into the prevalence and incidence of gastroparesis, identifying idiopathic and diabetic causes as the most common.
It also notes that patients with diabetic gastroparesis face a higher risk of mortality compared to those with idiopathic forms.
Ongoing clinical trials are exploring innovative treatments for gastroparesis, including:
These studies reflect a growing interest in unravelling the complexities of gastroparesis and developing more effective treatment modalities.
In wrapping up our exploration of gastroparesis, it’s clear that this condition predominantly affects women, particularly those over 30, and is significantly influenced by underlying health issues like diabetes and neurological disorders.
With causes ranging from idiopathic origins to complications from medications and surgeries, managing gastroparesis involves a multifaceted approach, including dietary changes, medications, and sometimes surgical interventions.
Looking ahead, continued research is crucial to unravel the complexities of gastroparesis, enhance treatment strategies, and ultimately improve patient outcomes. By deepening our understanding and refining our approaches, we can offer better support and solutions for those living with this challenging condition.
Q. Can gastroparesis be cured?
A. No, gastroparesis cannot be fully cured, but symptoms can be managed through diet, medications, and sometimes surgery.
Q. What foods should be avoided with gastroparesis?
A. High-fat and high-fiber foods should be avoided as they slow down digestion and can worsen symptoms.
Q. How is gastroparesis diagnosed?
A. Diagnostic methods include gastric emptying tests, upper endoscopy, and imaging tests to assess stomach motility.
Q. Can stress worsen gastroparesis symptoms?
A. Yes, stress and anxiety can aggravate gastroparesis symptoms by impacting digestion and stomach muscle function.
Q. Is gastroparesis a life-threatening condition?
A. While not typically life-threatening, complications like malnutrition, severe dehydration, and bezoars can lead to serious health issues.